Fluid Loss
Recall that when tissue is burned, an inflammatory response is activated. Part of this inflammatory response causes capillaries to become leaky. It is thought that there is also a cellular shift of sodium that also adds to the drastic loss of intravascular fluid. This loss of fluid from the intravascular space causes burn shock. Burn shock is a combination of hypovolemic, cardiogenic, and distributive shock. As fluids leave the intravascular space, the blood cells become very concentrated. Intravascular hypovolemia reaches maximum levels around twelve hours after the initial injury. Reduced cardiovascular efficiency is also a result of this fluid loss. The heart's ability to pump efficiently is reduced due to low decreased plasma volume, increased afterload (the for that the heart pumps against), and decreased cardiac contractility. Obviously, burn patients need to undergo aggressive resuscitation within the first minutes, hours, and days of their burn.Fluid Replacement
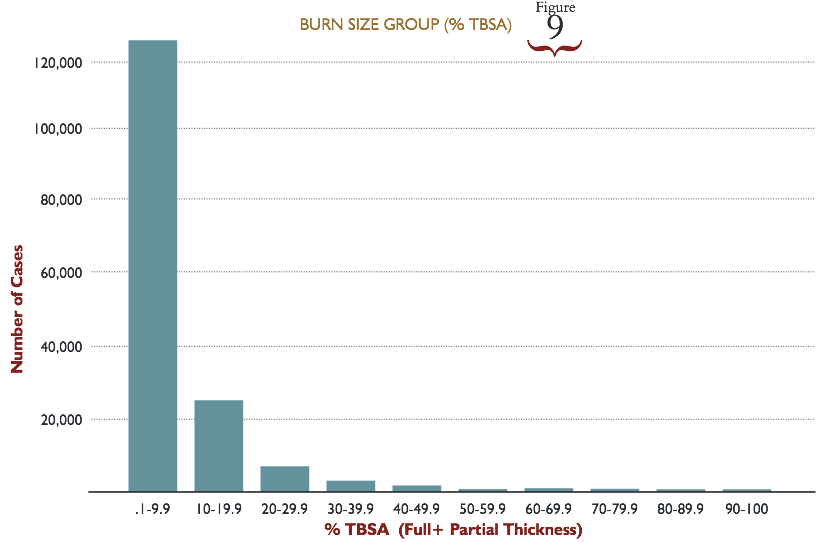
Burns that are less that 20% TBSA can be managed with oral resuscitation but intravascular resuscitation is more commonly done in the United States. Vomiting has become an issue for some burn patients when oral resuscitation has been attempted. Needless to say, for burns higher than 20% TBSA (and not involving the face), intravascular fluid resuscitation is the primary route of fluid replacement in the US. Numerous formulas are used to calculate the amount of fluid resuscitation that a burn patient may require. Typically, these formulas consider body weight and TBSA burned. Below are some of the more frequently formulas used, taken verbatim from Haberal, Sakallioglu Abali, and Karakayali's article titled, "Fluid management in major burn injuries (par 11-16)."Adult Burn Fluid Resuscitation Formulas
Parkland formula
- Initial 24 hours: Ringer’s lactated (RL) solution 4 ml/kg/% burn for adults and 3 ml/kg/% burn for children. RL solution is added for maintenance for children:
- 4 ml/kg/hour for children weighing 0–10 kg
- 40 ml/hour +2 ml/hour for children weighing 10–20 kg
- 60 ml/hour + 1 ml/kg/hour for children weighing 20 kg or higher
This formula recommends no colloid in the initial 24 hours. - Next 24 hours: Colloids given as 20–60% of calculated plasma volume. No crystalloids. Glucose in water is added in amounts required to maintain a urinary output of 0.5–1 ml/hour in adults and 1 ml/hour in children.
Modified Parkland formula
- Initial 24 hours: RL 4 ml/kg/% burn (adults)
- Next 24 hours: Begin colloid infusion of 5% albumin 0.3–1 ml/kg/% burn/16 per hour
Brooke formula
- Initial 24 hours: RL solution 1.5 ml/kg/% burn plus colloids 0.5 ml/kg/% burn plus 2000 ml glucose in water
- Next 24 hours: RL 0.5 ml/kg/% burn, colloids 0.25 ml/kg/% burn and the same amount of glucose in water as in the first 24 hours
Modified Brooke
- Initial 24 hours: No colloids. RL solution 2 ml/kg/% burn in adults and 3 ml/kg/% burn in children
- Next 24 hours: Colloids at 0.3–0.5 ml/kg/% burn and no crystalloids are given. Glucose in water is added in the amounts required to maintain good urinary output.
Evans formula (1952)
- First 24 hours: Crystalloids 1 ml/kg/% burn plus colloids at 1 ml/kg/% burn plus 2000 ml glucose in water
- Next 24 hours: Crystalloids at 0.5 ml/kg/% burn, colloids at 0.5 ml/kg/% burn and the same amount of glucose in water as in the first 24 hours
Monafo formula
Monafo
recommends using a solution containing 250 mEq Na, 150 mEq lactate and
100 mEq Cl. The amount is adjusted according to the urine output. In the
following 24 hours, the solution is titrated with 1/3 normal saline
according to urinary output.
Pediatric Burn Fluid Resuscitation Formulas
Shriner’s cincinnati
Initial 24 hours:
- For older children:Lactated Ringer’s (RL) solution 4 ml/kg/% burn +1500 ml/m2 total (1/2 of total volume over 8 hours, rest of the total volume during the following 16 hours)
- For younger children:4 ml/kg/% burn +1500 ml/m2 total, in the first 8 hoursRL solution + 50 mEq NaHCO3RL solution in the second 8 hours5% albumin in LR solution in the third 8 hours
Galveston
Initial 24 hours: RL 5000 ml/m2 burn + 2000 ml/m2 total (1/2 of total volume over 8 hours, rest of the total volume in 16 hours)
Some burn units, especially those specializing in pediatric burns, will adjust these formulas or use their own formula according to their expertise and the current situation.